Mammography Appointment Guide
What Is Mammography?
Mammography is specialized medical imaging that uses a low-dose x-ray system to see inside the breasts. A mammography exam, called a mammogram, aids in the early detection and diagnosis of breast diseases in women and men. X-ray exams assist physicians in diagnosing and
treating medical conditions. X-rays expose patients to a small dose of ionizing radiation to produce pictures of the inside of the body. X-rays are the oldest and most often used form of medical imaging.
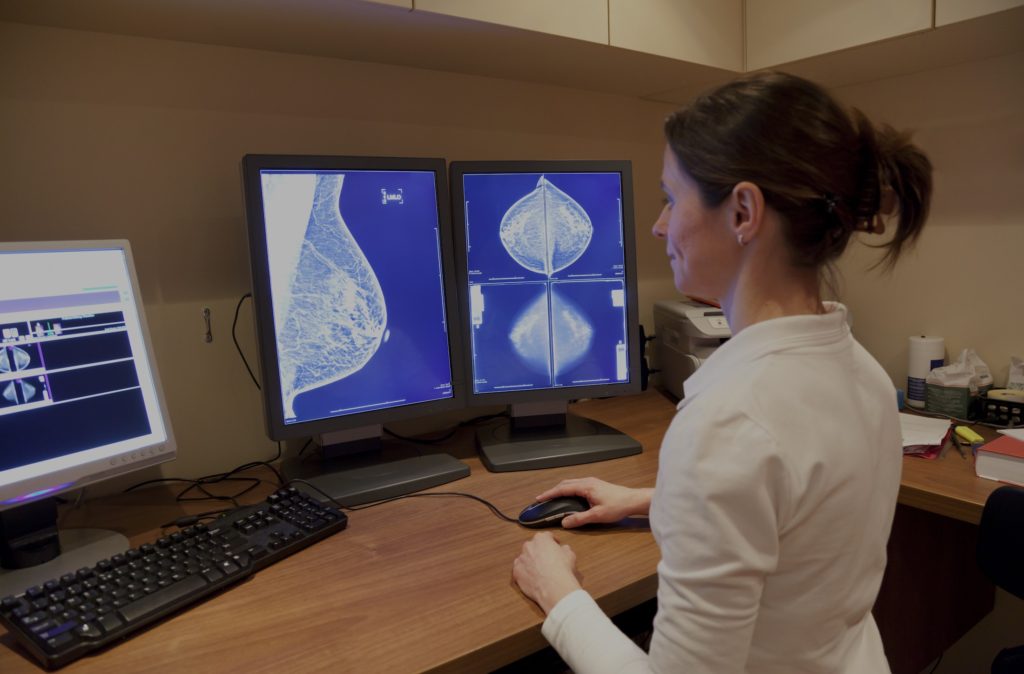

Digital mammography, also called full-field digital mammography (FFDM), is a mammography system in which the x-ray film is replaced by electronics that convert x-rays into mammographic pictures of the breast. Digital mammography enables better pictures with a lower radiation dose. These images of the breast are transferred to a computer for review by the radiologist and for long term storage.
Why Mammography?
Mammography remains the best screening test tool for most women (and occasionally men) to find breast cancer. Regular mammographs are the number one way to detect breast cancer early sometimes up to three years before it can be felt by the patient or physician. This test requires the removal of your clothes above the waist and changing into a hospital gown. Please do not wear any antiperspirant, deodorant, powder or cream on the day of your mammogram as these may appear on the mammogram and interfere with correct diagnosis. Tell your doctor about any breast symptoms or problems, prior surgeries, hormone use, whether you have a family or personal history of breast cancer, and if there’s a possibility you are pregnant. If possible, obtain copies of your prior mammograms and make them available to your radiologist on the day of your exam. Leave jewelry at home and wear loose, comfortable clothing.
Schedule Your Mammography Appointment Today
*Fields marked with an asterisk are mandatory.
What is a Mammogram used for?
Mammograms are used as a screening tool to detect early breast cancer in women experiencing no symptoms (when it is most treatable). They can also be used to detect and diagnose breast disease in women experiencing symptoms such as a lump, pain, skin dimpling or nipple discharge.
Screening Mammography
Mammography plays a central part in early detection of breast cancers because it can show changes in the breast years before a patient or physician can feel them. Current guidelines from the American College of Radiology (ACR) and the National Comprehensive Cancer Network (NCCN) recommend screening mammography every year for women, beginning at age 40. In Canada, annual mammography screening start for women at age 40. Cancer Care Ontario.
Research has shown that annual mammograms lead to early detection of breast cancers, when they are most curable and breast-conservation therapies are available.
The ACR and the National Cancer Institute (NCI) also suggest that women who have had breast cancer, and those who are at increased risk due to a family history of breast or ovarian cancer, should seek expert medical advice about whether they should begin screening before age 40 and the need for other types of screening. If you are at high risk for breast cancer, you may need to obtain a breast MRI in addition to your annual mammogram.
Screening remains the primary way to the early detection of breast cancer. Annual screening mammography is currently recommended by most National organizations for all women over the age of 40. Approximately 10% of women who undergo screening mammography, we will be recalled for additional views. If you are recalled, this should not cause undue worry as 9 out of 10 patients who are recalled for additional views are subsequently categorized as benign or probably benign.
If additional views are necessary, you ill be contacted and scheduled directly by the clinic on behalf of your physician. If a biopsy is required, you will be referred for biopsy. Your physician can assist with coordinating the best location to obtain this procedure which is mainly done at hospitals currently.
Diagnostic Mammography
Diagnostic mammography is used to evaluate a patient with abnormal clinical findings—such as a breast lump or nipple discharge—that have been found by the woman or her doctor. Diagnostic mammography may also be done after an abnormal screening mammogram in order to evaluate the area of concern on the screening exam.
Mammogram vs Breast Ultrasound - Understanding the Difference
Breast imaging is the examination of the breast to demonstrate any changes and abnormalities using mammography and/or ultrasound.
A mammogram is an x-ray test of the breast tissue. It can provide information about lumps, calcifications and other abnormalities that may be present in the breast. It is also available for screening purposes for women without any breast problems.
Breast ultrasound uses sound waves – not radiation – to show breast tissue. A breast ultrasound can show areas of the breast, including the areas closest to the chest wall that are difficult to see in a mammogram. Breast ultrasound is used to check any abnormalities in the breast and provide further information.
Ontario Breast Screening Program (OBSP)
 Our breast imaging centre at Valence Medical Imaging is working towards becoming an Ontario Breast Screening Program (OBSP) assessment site as part of our initiative to partner Cancer Care Ontario. The OBSP is a self-referral screening mammogram that does not require a requisition from your family doctor. This program is for Ontario women only, aged 40 to 74 years old, who have no previous history of breast cancer, no implants and no current breast symptoms.
Our breast imaging centre at Valence Medical Imaging is working towards becoming an Ontario Breast Screening Program (OBSP) assessment site as part of our initiative to partner Cancer Care Ontario. The OBSP is a self-referral screening mammogram that does not require a requisition from your family doctor. This program is for Ontario women only, aged 40 to 74 years old, who have no previous history of breast cancer, no implants and no current breast symptoms.
Women aged 40-74 are eligible for a mammogram provided by the Ontario Breast Screening Program (OBSP) every 2 years. In screening cases, a doctor’s referral is not required. For patients presenting with new breast symptoms, breast implants or a history of malignant tumours, a physician’s referral is required.
If you are 40 to 49 years old, talk to your doctor about your risk for breast cancer, along with the benefits and limitations of having a mammogram. If you are over 74 years old, speak with your health care provider about getting tested for breast cancer. If you choose to get tested you will need a referral for a mammogram from your doctor or nurse practitioner.
If you do not have a doctor or a nurse practitioner, you can find one through Health Care Connect at 1-800-445-1822.
The Ontario Breast Screening Program (OBSP) screens women ages 30 to 69 who are confirmed to be at high risk of developing breast cancer, once a year with a mammogram and breast magnetic resonance imaging (MRI) (or screening breast ultrasound if MRI is not medically appropriate). This kind of testing is based on scientific evidence and ensures that high risk women receive the benefits of organized screening.
Who is Eligible through the High-Risk OBSP?
Ontario women ages 30 to 69 can get screened through the High Risk OBSP if they have a referral from their doctor, a valid Ontario Health Insurance Plan number, no acute breast symptoms, and fall into one of the following risk categories:
- Are known to have a gene mutation that increases their risk for breast cancer (e.g.BRCA1, BRCA2, TP53, PTEN, CDH1)
- Are first-degree relatives (parent, brother, sister or child) of someone who has a gene mutation that increases their risk for breast cancer (e.g. BRCA1, BRCA2, TP53, PTEN, CDH1), have already had genetic counselling and have chosen not to have genetic testing.
- Have been assessed by a genetics clinic (using the IBIS or BOADICEA tools) as having a 25% or greater lifetime risk of breast cancer based on personal family history.
- Have had radiation therapy to the chest to treat another cancer or condition (e.g., Hodgkin lymphoma) before age 30 and at least 8 years ago.
Risk for breast cancer is divided into 3 broad categories:
Average Risk: Women with 10-15% lifetime risk of cancer.
Most women fall in this category if:
- There is no personal or first degree relative with a history of breast cancer and,
- Not dense breasts on mammography.
Intermediate Risk: Women with 15-20% lifetime risk of cancer.
This is the next big category if:
- Personal history of breast cancer after age 50.
- First degree relative with a history of breast cancer.
- Dense breasts on mammography.
High Risk: Women with greater than 20% lifetime risk of cancer.
This is the category that requires the closest monitoring:
- Personal history of breast cancer before age 50, or
- There is BRCA genetic mutation, or
- History of radiation treatment to the chest between age 10 to 30.
Mammogram Preparations
The best time to book your mammogram procedure is one week following your period to reduce breast sensitivity. Try not to have your mammogram the week before your get your period or during your period. Your breasts may be tender or swollen during that time. The best time for a mammogram is one week following your period. Always inform your doctor or x-ray technologist if there is any possibility that you are pregnant.
On the day of the study, wear comfortable clothing and do not wear deodorant, talcum powder, perfume or lotion under your arms. These products can show up as spots on your images.
You will need to undress form your waist up for the mammogram.
This test requires the removal of your clothes above the waist and changing into a hospital gown. Please do not wear any antiperspirant, deodorant, powder or cream on the day of your mammogram.
What does having a mammogram feel like?
Having a mammogram is uncomfortable for most women and some women find it painful. A mammogram takes only a few moments and the discomfort is over soon. What you feel depends on the skill of the technologist, the size of your breasts, and how much they need to be pressed. Your breasts may be more sensitive if you are about to get or have your period. A doctor with special training, called a radiologist, will look at the X-ray for early signs of breast cancer or other problems.
What does the mammography equipment look like?
A mammography unit is a box with a tube that produces x-rays. The unit is used exclusively for breast x-ray exams and features special accessories to limit x-ray exposure to only the breast. The unit features a device to hold and compress the breast and position it so the technologist can capture images at different angles.
How does the mammography procedure work?
X-rays are a form of radiation like light or radio waves. X-rays pass through most objects, including the body. The technologist carefully aims the x-ray beam at the area of interest. The machine produces a small burst of radiation that passes through your body. The radiation records an image on photographic film or a special detector.
Different parts of the body absorb the x-rays in varying degrees. Dense bone absorbs much of the radiation while soft tissue (muscle, fat, and organs) allows more of the x-rays to pass through them. As a result, bones appear white on the x-ray, soft tissue shows up in shades of gray, and air appears black.
Most x-ray images are electronically stored digital files. Your doctor can easily access these stored images to diagnose and manage your condition.
How is the procedure performed?
During mammography, a specially qualified radiologic technologist will position your breast in the mammography unit. Your breast will be placed on a special platform and compressed with a clear plastic paddle. The technologist will gradually compress your breast. You will feel some pressure.
Breast compression is necessary in order to:
- Even out the breast thickness so that all of the tissue can be visualized.
- Spread out the tissue so that small abnormalities are less likely to be hidden by overlying breast tissue.
- Allow the use of a lower x-ray dose since a thinner amount of breast tissue is being imaged.
- Hold the breast still in order to minimize blurring of the image caused by motion.
- Reduce x-ray scatter to increase sharpness of picture.
You will be asked to change positions between images. The routine views are a top-to-bottom view and an angled side view. The process will be repeated for the other breast. During screening breast tomosynthesis, two-dimensional images are also obtained or created from the synthesized 3-D images.
You must hold very still and may need to hold your breath for a few seconds while the technologist takes the x-ray. This helps reduce the possibility of a blurred image. The technologist will walk behind a wall or into the next room to activate the x-ray machine.
When the examination is complete, the technologist may ask you to wait until the radiologist confirms they have all the necessary images and the images do not need to be retaken. The technologist is not able to provide you with the results of the mammogram. Each patient’s mammogram may look a little different because all breasts are a different.
The examination process should take about 30 minutes.
What will I experience during and after the procedure?
You will feel pressure on your breast as it is squeezed by the compression paddle. Some women with sensitive breasts may experience discomfort. If this is the case, schedule the procedure when your breasts are least tender. Be sure to inform the technologist if pain occurs as compression is increased. If discomfort is significant, less compression will be used. Always remember compression allows better quality mammograms.
Who interprets the results and how do I get them?
A radiologist, who is a doctor trained to supervise and interpret radiology examinations, will analyze the images. The radiologist will send a signed report to your primary care physician who will discuss the results with you.
You will also be notified of the results by the mammography facility.
You may need a follow-up exam. If so, your doctor will explain why. Sometimes a follow-up exam further evaluates a potential issue with more views or a special imaging technique. It may also see if there has been any change in an issue over time. Follow-up exams are often the best way to see if treatment is working or if a problem needs attention.
What are the benefits vs. risks?
Benefits
- Screening mammography reduces the risk of death due to breast cancer. It is useful for detecting all types of breast cancer, including invasive ductal and invasive lobular cancer.
- Screening mammography improves a physician’s ability to detect small tumors. When cancers are small, the woman has more treatment options.
- The use of screening mammography increases the detection of small abnormal tissue growths confined to the milk ducts in the breast, called ductal carcinoma in situ (DCIS).
- No radiation stays in your body after an x-ray exam.
- X-rays usually have no side effects in the typical diagnostic range for this exam.
Risks
- There is always a slight chance of cancer from excessive exposure to radiation. However, given the small amount of radiation used in medical imaging, the benefit of an accurate diagnosis far outweighs the associated risk.
- The radiation dose for this procedure varies.
- False Positive Mammograms. Five percent to 15 percent of screening mammograms require more testing such as additional mammograms or ultrasound. Most of these tests turn out to be normal. If there is an abnormal finding, a follow-up or biopsy may have to be performed. Most of the biopsies confirm that no cancer was present. It is estimated that a woman who has yearly mammograms between ages 40 and 49 has about a 30 percent chance of having a false-positive mammogram at some point in that decade and about a 7 percent to 8 percent chance of having a breast biopsy within the 10-year period.
- Women should always tell their doctor and x-ray technologist if they are pregnant.
Minimizing Radiation Exposure
Doctors take special care during x-ray exams to use the lowest radiation dose possible while producing the best images for evaluation. National and international radiology protection organizations continually review and update the technique standards radiology professionals use.
Modern x-ray systems minimize stray (scatter) radiation by using controlled x-ray beams and dose control methods. This ensures that the areas of your body not being imaged receive minimal radiation exposure.
Technologists follow the ALARA principle at all times. ALARA stands for “as low as reasonably achievable”. ALARA means avoiding exposure to radiation that does not have a direct benefit to you, even if the dose is small.
How Long does it take to get results?
You will usually get the results within a few days to a week. A radiologist reads your mammogram and then reports the results to you and your doctor. If there is a concern, you will hear from the facility earlier. Contact your health care provider or the mammography facility if you do not receive a report of your results after 1 week.
Understanding your results and follow-up
Normal Results
If your results come back as normal, you will continue to get mammograms according to recommended time intervals. Mammograms work best when they can be compared with previous ones. This allows the radiologist to compare them to look for changes in your breasts.
Abnormal Results
An abnormal mammogram does not always mean that there is cancer. But you will need to have additional mammograms, tests, or exams before the doctor can tell for sure. You may also be referred to a breast specialist or a surgeon. It does not necessarily mean you have cancer or need surgery. These doctors are experts in diagnosing breast problems. Doctors will do follow-up tests to diagnose breast cancer or to find that there is no cancer.
What are the limitations of mammography?
Mammography remains the best screening tool for breast cancer available today, but mammograms do not detect all breast cancers. This is called a false negative result. On the other hand, when a mammogram looks abnormal and no cancer is present, this is called a false-positive result.
Screening mammographic images themselves are often not enough to determine the existence of a benign or malignant disease with certainty. If there are abnormalities, your radiologist may recommend further diagnostic studies.
It is very important to understand that not all breast cancers can be seen on mammography. Interpretations of mammograms can be difficult because a normal breast looks different for each woman. Also, the appearance of an image may be compromised if there is powder or salve on the breasts or if you have undergone breast surgery. Because some breast cancers are hard to visualize, a radiologist may want to compare the image to views from previous examinations.
Increased breast density has attracted attention from a number of state legislatures and more recently the federal government for multiple reasons, including:
- Increased breast density makes it difficult to see a cancer on mammography.
- Increased breast density may increase the risk of getting breast cancer.
The radiologist reading your mammogram determines your breast density and reports it to your doctor.
Breast implants can also impede accurate mammogram readings because both silicone and saline implants are not transparent on x-rays and can block a clear view of the tissues around them, especially if the implant has been placed in front of, rather than beneath, the chest muscles. Experienced technologists and radiologists know how to carefully compress the breasts to improve the view without rupturing the implant.
Research is being done on a variety of breast imaging techniques that can contribute to the early detection of breast cancer and improve the accuracy in distinguishing non-cancerous breast conditions from breast cancers.

