Southern Ontario's Leading
Medical Imaging Provider
For Over 35 Years.
Call us today for Information.








Welcome To
Valence Medical Imaging
Ultrasound X-Ray Clinic Toronto
We are a family owned and operated diagnostic medical imaging practice. For over 35 years, we have been providing leading-edge digital x-ray, ultrasound and bone density imaging services to Southern Ontario communities.
Our patients’ comfort and care are our primary concern. From the moment you make an appointment, to your visit, to the time you receive your results, we pay attention to every detail to ensure as stress-free an experience as possible.



As of October 8, 2024, the Ontario Breast Screening Program (OBSP) has expanded the age range and allows individuals aged 40 – 74 to self-refer for publicly funded mammograms, eliminating the need for a doctor’s referral.
Breast cancer screening, particularly through mammograms, is crucial for early detection, which significantly improves treatment outcomes and survival rates. Early detection allows for less invasive treatment options and a higher chance of successful recovery.
Book your appointment today:
40 Finchgate Blvd., Suite 320, Bramalea, ON L6T 3J1
· No doctor’s referral needed
· No requisition needed
· Same day appointments available
· Get all your medical imaging done in one convenient location
· Don’t pay for parking, give your license plate number to the receptionist for free parking.
Call or book online.
We’re proud of servicing the Toronto, Niagara, Whitby, Brampton, Bramalea and GTA for the last 35 years. With outstanding medical imaging services from Ultrasound X Ray Clinic Toronto, Bone Mineral Densitometry (BMD) and Fluoroscopy.
Please complete the Quick Form below. After you submit this information, CDN support will contact you to confirm your appointment. If you have a medical emergency, dial 911.
Short Wait times
Short wait times to book appointments
Fast Report Times
Fast 24-hour report turnaround time
Fast STAT Turnarounds
STAT report turnaround in less than an hour
Electronic PDF's
Electronic PDFs of requisitions
3rd Party Coverage
3rd party/WSIB/Private Pay/Chiropractors
Specialized Radiologists
Sub-specialized radiologists
Short Wait times
Short wait times to book appointments
Fast Report Times
Fast 24-hour report turnaround time
Fast STAT Turnarounds
STAT report turnaround in less than an hour
Electronic PDF's
Electronic PDFs of requisitions
3rd Party Coverage
3rd party/WSIB/Private Pay/Chiropractors
Specialized Radiologists
Sub-specialized radiologists
I had a tech named Ann and she was amazing! The entire time she was reassuring. My comfort and dignity was always clearly very important to her. She made me feel very comfortable, respected and I left feeling that exam was geared to me and my needs. Anne is very good at what she does.
Finchgate
Very experienced staff, extremely understanding and assuring technologist. Thank you!
Heartlake
Wonderful office, great service, very clean
Finchgate
The clinic is a real gem, so clean and all the staff are professional. Five stars!
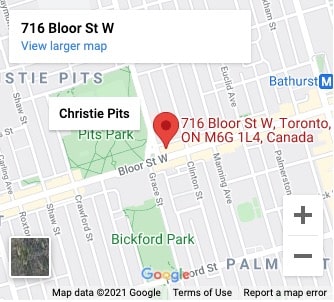
Bloor Christie
Had X-rays today and the staff were so friendly and efficient.
Whitby
I had the good fortune to see your staff at work - they should be commended. Aman and Kunnalee were so courteous and professional during my visit. Everyone should keep up the good work.
Heartlake
This clinic is so much better than the other places I have had imaging. It is clean, the staff are professional and I got my results so quickly. Thank you!
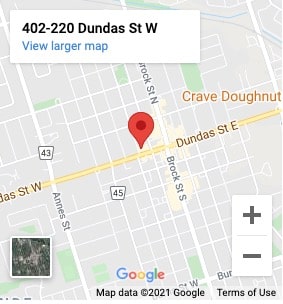
Lawrence Bathurst
Seven convenient locations within the Toronto, GTA, Brampton, Whitby and Niagara Falls. Book your appointment for Ultrasound X Ray Clinic Toronto Today.

- 508 Lawrence Ave. W. #25B North York, ON M6A 1A1
- 416-787-0229
- 416-787-0220

- 2374 Eglinton Ave. E. Lower Level Scarborough, ON M1K 2P4
- 416-757-8497
- 416-757-4146
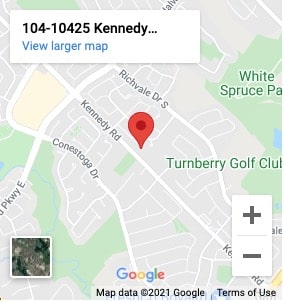
- 10425 Kennedy Road North Suite 104 Brampton, ON L6Z 0A4
- 905-846-7733
- 905-846-5414

- 40 Finchgate Blvd. Suite 320 Bramalea, ON L6T 3J1
- 905-792-8440
- 905-792-0806
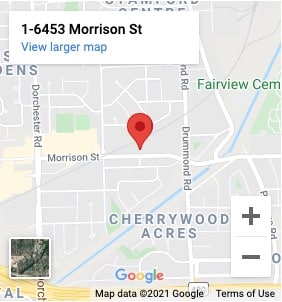
- 6453 Morrison Street Suite 1 Niagara Falls, ON L2E 7H1
- 905-374-1686
- 905-374-4950

Can You Travel Outside Ontario and Still Use OBSP? What Patients Need to Know
If you live in Ontario and rely on the Ontario Breast Screening Program for routine mammograms, travel can raise a real, practical question: can you

What Are the Benefits of Joining OBSP Early? A Complete Ontario Screening Guide
If you’re thinking about breast screening in Ontario, timing matters more than most people realize. In our experience working with women across Brampton and Bramalea,

How to Encourage a Loved One to Join OBSP: A Supportive Guide for Ontario Families
We’ve worked with families across Brampton and Bramalea who all want the same thing: peace of mind. OBSP awareness often starts at the kitchen table,